Vaccines now in clinical trials can raise broad-spectrum antibodies against more than one form of hemagglutinin and provide protection against the flu strains that have been most troublesome from a public health perspective.
And the advances in structural biology and vaccinology that underpin the work could be applied to other rapidly mutating viruses, including SARS-CoV-2.
Although SARS-CoV-2 does not mutate as rapidly as the flu virus, the brand-new vaccines against it are already less effective against some of the variants that have evolved since the virus first came to the attention of public health officials roughly 15 months ago. Some researchers claim that either repeat vaccinations against new variants or the development of vaccines that can more broadly neutralize SARS-CoV-2, and ideally, other coronaviruses, will be necessary to keep the upper hand over COVID-19.
In January, researchers at the California Institute of Technology reported in Science that they were able to induce antibodies to multiple different strains of coronavirus by presenting fragments of spike protein from different coronavirus strains.
Even if annual flu, or COVID-19, vaccines still needed to be developed in addition to a broadly neutralizing vaccine, "if you had a safety net... it would allow you greater consistency and greater efficacy that could provide a tremendous amount of benefit from a public health perspective," Gary Nabel told BioWorld Science.
In the March 3, 2021, issue of Science Translational Medicine, Nabel and his colleagues published primate data showing that vaccination with a mix of two stabilized headless hemagglutinins offered broad-spectrum protection against influenza virus infection from strains with hemagglutinins of the type H1 and H3.
The research was performed while Nabel was chief scientific officer of Sanofi US, which owns the intellectual property related to the work. He is currently the co-founder and CEO of Natick, Massachusetts-based startup Modex Therapeutics.
Although there are dozens of different hemagglutinin forms, strains with the H1 and H3 forms have an outsize impact on human health. Three of the past four influenza pandemics, the 1918, 1957 and 2009 pandemics, were caused by flu strains whose hemagglutinin was type H1 or H3. And in animal models, Nabel and his colleagues have shown that the stabilized-stem vaccines were also effective against H5-type viruses, a group that includes several avian flu strains, including H5N1 and the H5N8 strain that has recently infected poultry workers in Russia.
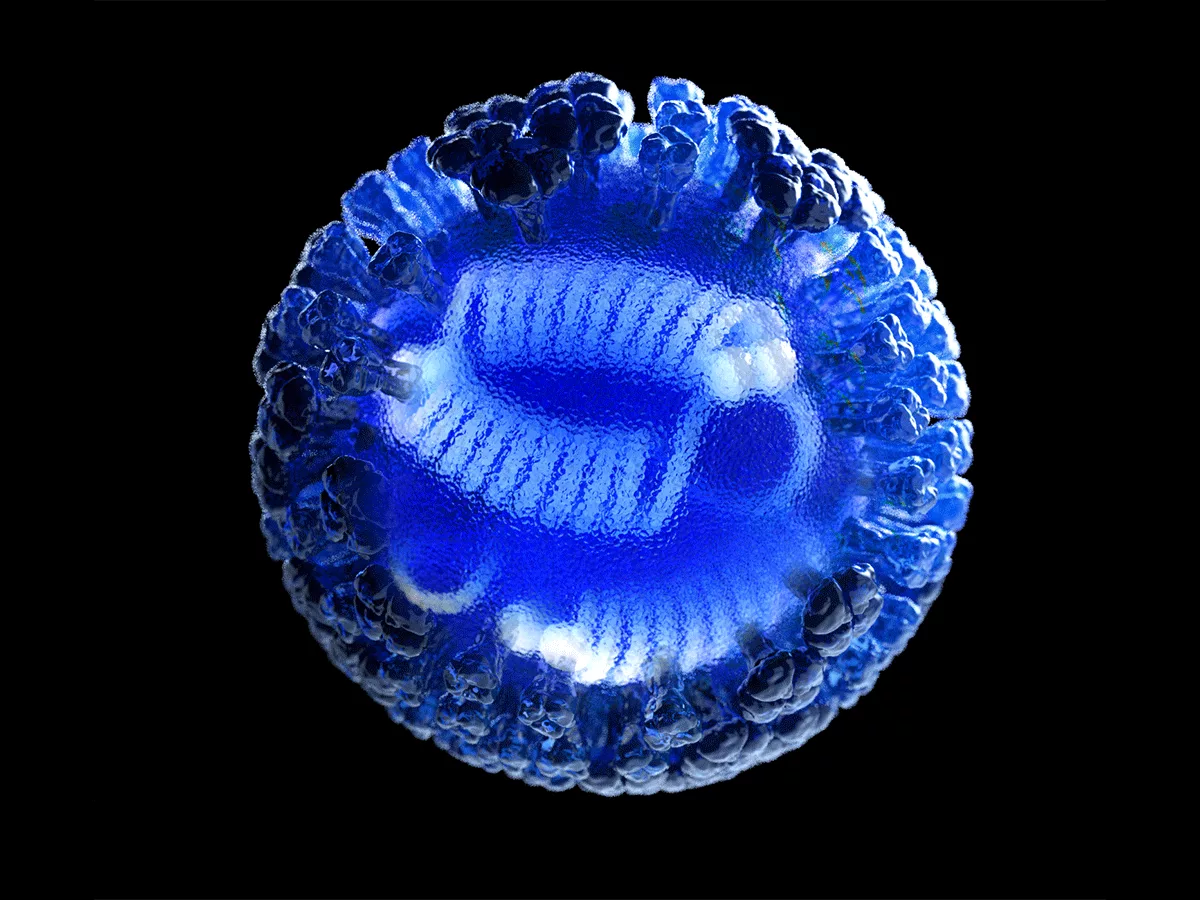
The trials are testing a form of hemagglutinin that is missing the protein's "head" structure, which is the most obvious part of hemagglutinin to the immune system, but one that mutates rapidly. Removing the head makes an invariant part of hemagglutinin, the stalk, visible to the immune system, leading to the production of broadly neutralizing antibodies.
The studies are a continuation of work reported in 2015, when Nabel and his colleagues reported that headless hemagglutinin could provide broad-spectrum protection against H1 influenza viruses in mice and ferrets.
The new paper added H3 into the mix, which broadens protection to include the group B influenza viruses, and showed that the vaccine was effective in primates.
The earlier lack of primate data had led to skepticism from some quarters that the approach could succeed in the clinic, Nabel recounted. "The reason we never looked in monkeys is that one of the germline genes that we think is critical for the human immune response is mutated in the monkey... There's a disparity in a critical immune component."
Other vaccine studies, however, suggested that an adjuvanted version of the vaccine might be successful in primates, and "we decided that maybe we should just do the experiment," he said, "And the short version is that it worked very well, better than we had ever anticipated... We realized that we were getting remarkably broad protection."
Both the vaccine used in the Science Translational Medicine paper and another vaccine that has used the same engineering principles to create a headless hemagglutinin from the H10 group are currently in clinical trials. There are two dozen hemagglutinin forms across influenza group A and B, and the vaccines are unlikely to be fully protective against all of them. But the advances in vaccinology that are enabling the development of broad-spectrum vaccines against rapidly mutating viruses still have their limits, Nabel said: "You find a balance between what you are most concerned about and the ones that are actually circulating, and you build your approach from there."