A multicenter study led by scientists at Monash Institute of Pharmaceutical Sciences (MIPS) in Melbourne, Australia, has described a new mesenteric lymph vessel-based pathogenic mechanism, which was shown to contribute to visceral fat accumulation and insulin resistance (IR) in both mice and humans.
Reported in the September 20, 2021, edition of Nature Metabolism, the study also demonstrated the potential to treat metabolic diseases through normalizing mesenteric lymphatic function via pharmacologic intervention in mice fed a high-fat diet (HFD).
"Our work builds on studies showing that obesity is associated with significant impairments in lymphatic function in peripheral tissues, and that fat tissue accumulates around the site of lymph leakage in humans and mice with dysfunctional lymphatics," said study co-leader Natalie Trevaskis, an associate professor at MIPS.
However, "ours is the first study to establish that dysfunctional mesenteric lymphatics, particularly the leakage of mesenteric lymph into surrounding fat tissue, promotes fat accumulation and IR, and that this can be targeted to treat metabolic diseases," said Trevaskis.
High weight is "predominantly driven by modern diet and a sedentary lifestyle, but genetics, hormonal, physiological and environmental factors also play a role," she told BioWorld Science.
Among these factors, "our study focused on obesity-associated lymphatic vascular dysfunction and how this causes IR and can be targeted to treat IR and T2DM [type 2 diabetes mellitus], rather than treating obesity per se."
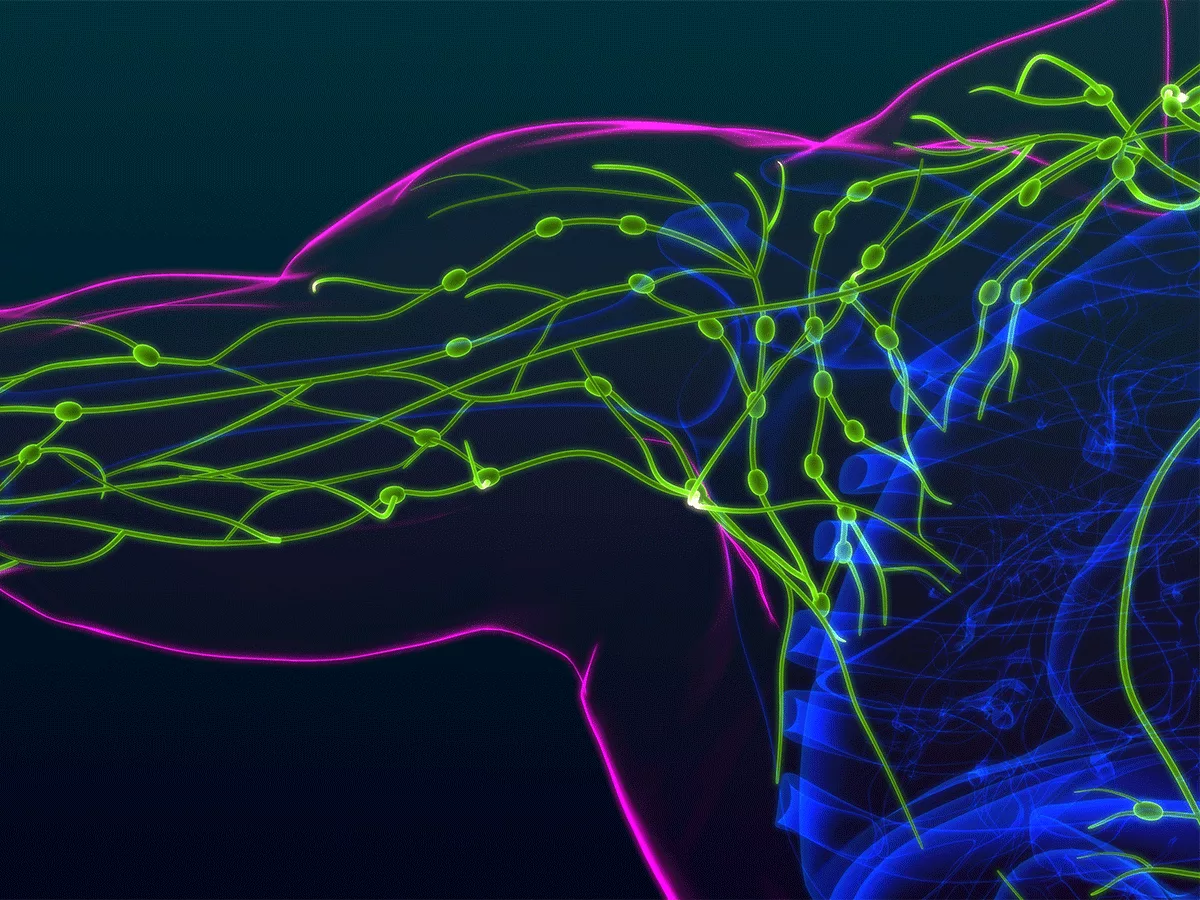
Lymphatic vasculature
The lymphatic vasculature is essential for dietary lipid absorption, fluid homeostasis and immunity, while contributing to the pathogenesis of cancers, inflammatory diseases and neurodegenerative diseases.
Blocking dietary lipid transport via the lymphatic systems in intestinal villi was recently shown to protect against obesity, although whether the mesenteric lymphatics contribute to adipose tissue inflammation and metabolism and IR remains unclear.
However, obesity is associated with significantly impaired lymphatic function in peripheral tissues, and adipose tissue accumulates around the site of lymph leakage in lymphedema patients and in transgenic mice with abnormal lymphatics.
Excessive accumulation of visceral apidose tissue (VAT), which enfolds internal organs and mesenteric lymphatics draining the gut, leads to excess VAT release of fatty acids and adipokines, promoting IR in gluco-regulatory tissues.
Conversely, accumulation of subcutaneous adipose tissue (SAT), which is associated with subcutaneous peripheral lymphatics, is not a risk factor for IR.
Importantly, circulating VAT mesenteric lymph fluid is enriched in gut-derived lipid metabolites and proinflammatory mediators, compared with peripheral SAT lymph fluid.
Moreover, mesenteric lymphatic vessel permeability and contractility are altered in genetically modified diabetic mice and rats fed a high-fructose diet.
Previous research has also established that inherent permeability of mesenteric and peripheral collecting lymphatic vessels enables distribution of lymph components to surrounding adipose tissue.
Thus the MIPS researchers hypothesized that mesenteric lymphatic dysfunction, particularly leakage of HFD-modified mesenteric lymph into VAT, might promote VAT accumulation and IR.
Co-led by Trevaskis, MIPS director and professor Christopher Porter and postgraduate student Enyuan Cao, the Nature Metabolism study showed that mesenteric lymphatics became profoundly dysfunctional during progression of HFD-induced obesity in mice and humans.
Notably, they found that lymph from HFD-fed mice and humans stimulated lymphatic vessel growth, leading to formation of mesenteric lymphatic vessels that 'leaked' HFD-lymph into VAT, thereby promoting IR.
"We showed that lymph fluid promoted proliferation and migration of lymphatic endothelial cells in vitro when lymph was added during cell growth," explained Trevaskis.
"Using confocal imaging, we also showed that mesenteric lymphatic vessels in HFD-fed obese mice and in obese humans were disorganized and highly branched, then used live imaging techniques to visualize lymph leakage into surrounding fat."
The researchers then demonstrated that proinflammatory cyclo-oxygenase-2 (COX-2) and vascular epithelial growth factor C (VEGF-C) signaling via VEGF receptor 3 (VEGFR3) regulated obesity-associated mesenteric lymphatic dysfunction.
"VEGF-C signaling via VEGFR3 is the most important mediator of lymphangiogenesis in development and disease," Trevaskis said.
In addition, "prostaglandin E2 (PGE2) synthesized by the COX-2 enzyme has previously been shown to regulate lymphangiogenesis in cancer by recruiting or stimulating VEGF-C release from macrophages," she noted.
"To demonstrate that COX-2-PGE2 and VEGF-C-VEGFR3 signaling regulate obesity-associated mesenteric lymphatic dysfunction, we first confirmed in vitro that lymphatic endothelial cell migration induced by HFD lymph was inhibited by a COX-2 inhibitor, a VEGFR3 kinase inhibitor and an antagonist of the prostaglandin EP4 receptor."
Importantly, lymph-targeted inhibition of COX-2 using a glyceride prodrug of the COX-2 inhibitor, celecoxib, was shown to effectively reverse mesenteric lymphatic dysfunction and improve obesity and glycemic control.
"Celecoxib is used to treat inflammatory conditions such as arthritis, but we found that it was not completely effective in reversing mesenteric lymphatic dysfunction, obesity and insulin resistance," said Trevaskis.
Therefore, "we designed a glyceride prodrug of celecoxib to boost mesenteric lymphatic uptake and local accumulation of celecoxib to reduce mesenteric lymphatic dysfunction," she said.
"We found that the celecoxib prodrug did not reduce total body weight in HFD-fed obese mice but blocked their continued weight gain such that it matched that of normal control mice, while restoring glycemic control in the obese mice."
Together, these findings suggest that mesenteric lymphatic dysfunction contributes to visceral obesity and IR, thereby revealing targeted restoration of mesenteric lymphatic function as a potential treatment strategy for obesity and related metabolic diseases.
Looking ahead, Trevaskis noted that the glyceride celecoxib prodrug has not been approved for human use, "so will require extensive preclinical safety testing prior to entering clinical trials for obesity and metabolic diseases.
"Our group is also interested in investigating the impact of lymphatic dysfunction in a range of metabolic and inflammatory disease and cancers, while testing our lymph-targeted prodrug approach to treating these diseases."