A number of possible mechanisms have been explored, but there is still no safe, reliable and universally applicable method for delivering drugs across the blood-brain barrier (BBB) to treat central nervous system diseases.
Now researchers have succeeded in tuning the effect of methamphetamine (Meth), a cause of BBB breakdown, enabling brain penetration of small molecules and therapeutic proteins, without damaging the epithelial cells that constitute the main physical element of the barrier.
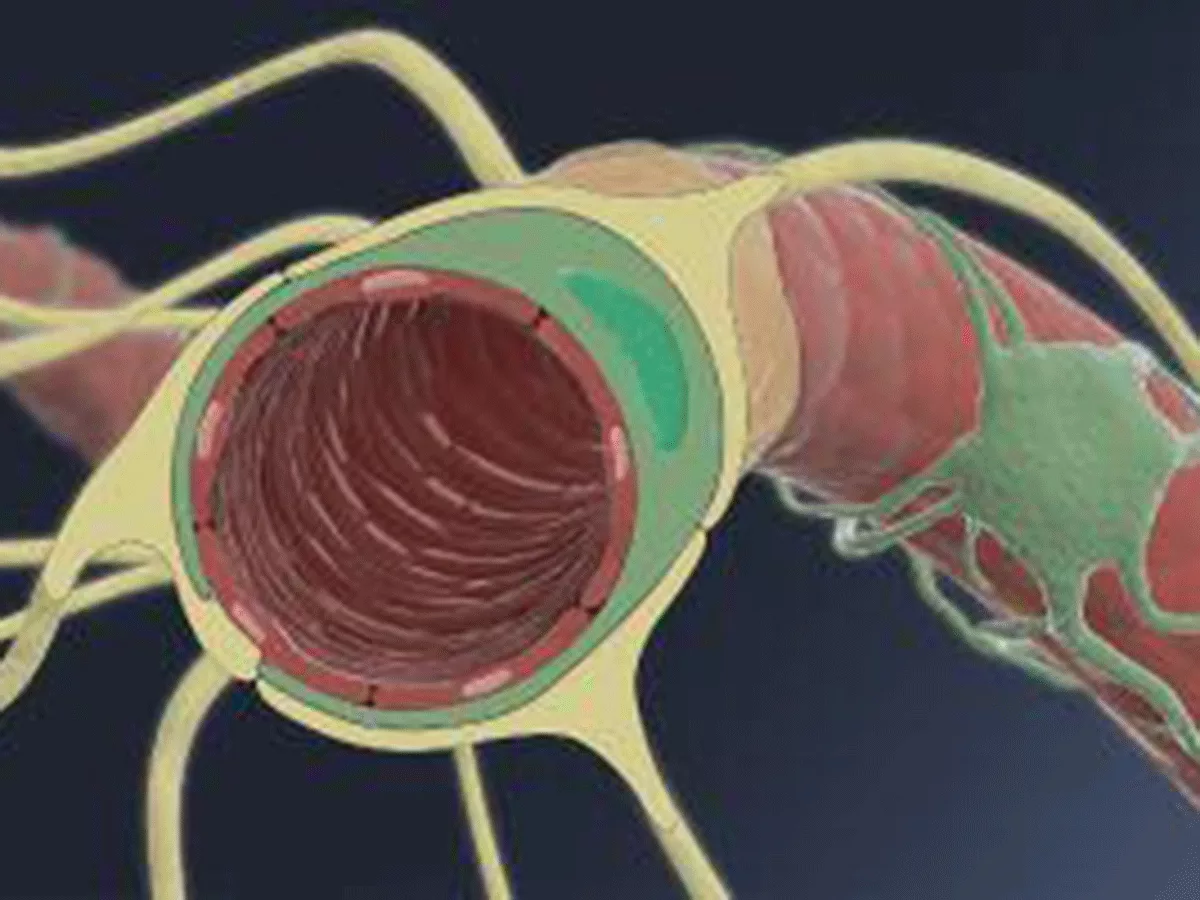
In a proof-of-principle study published in Cell Reports Medicine on January 11, 2022, the researchers showed how Meth rapidly induced the formation of cavities, or caveolae, in endothelial cells, triggering the transport of proteins and small molecules. They say this process could be harnessed to deliver drugs in the blood stream across the BBB.
"Our approach exploits the fact that caveolae are not normally expressed at a functional BBB," said co-author Patric Turowski, professor of vascular signaling at the Faculty of Brain Sciences, University College London. "We show that [caveolae] can be induced pharmacologically -- which is new -- using Meth, and that they are transport competent -- this is also new," he told BioWorld Science.
Using caveolae as carriers will have a safety advantage over other approaches to opening a passageway between the blood and the brain by disrupting the integrity of the BBB, for example, by loosening the tight junctions endothelial cells form with each other.
In contrast, induction of transport-competent caveolae at the BBB allows transport of blood constituents to the brain parenchyma without creating a direct connection between blood and brain, and thus "displays much lower toxicity for neuronal networks and, in particular, their delicate ionic environment," the researchers say.
The method also promises to be more straightforward than receptor-mediated delivery via transferrin or other specialists receptors that naturally control the entry of nutrients to the brain, since using these routes requires drugs to be coupled to a vector.
Low-dose Meth induces significant BBB leakage in rodents ex vivo and in vivo, but the effect is transitory and tight junctions remain intact, Turowski said. "[It] does not create a direct connection between blood and brain, and does not require vectorization of the drug to be transported. This latter aspect should make this approach very versatile for rapid, preclinical testing of experimental drugs."
The dose makes the poison, even for methamphetamine
The researchers established that concentrations of around 1 mcM Meth are sufficient to induce transport competent caveolae at the BBB. While this is lower than would be experienced by someone abusing Meth, it is at the top end, or just beyond what is reached by the only FDA-approved version of Meth, Dexoxsyn (methamphetamine hydrochloride), which is used for treating attention deficit hyperactivity disorder and obesity.
"We believe that a carefully designed protocol with maximum blood concentration of 1 mcM would be acceptable in terms of some mild and transient side effects, especially when applied in the context of devastating terminal diseases, such as glioblastoma," Turowski said.
The dose of Meth required is the same for small-molecule or protein drugs, with the researchers demonstrating the efficient transport of the chemotherapeutic doxorubicin, which has generally poor BBB permeability, and of a large protein, the vascular endothelial growth factor inhibitor aflibercept.
It also was shown that this method of delivery is controllable, Turowski said. "In our in vivo experiments, BBB opening occurred only following the initial 5 hours of Meth application, indicating normalization of the BBB thereafter," he said.
As a test of the potential clinical relevance, the researchers looked to see if Meth enhanced the efficacy of doxorubicin in a mouse model of glioma, finding there was a significant difference in survival between mice receiving doxorubicin alone compared to doxorubicin plus Meth. Median survival in the doxorubicin alone group was 17.5 days, compared to 22 days in the Meth group.
Post mortem investigation showed that satellite lesions outside the main bulk tumor area were significantly less frequent and smaller in size in the Meth treated mice.
In theory, the work is directly applicable to humans, since Meth is FDA approved. Indeed, the research was funded in part by the research charity Cancer Research UK through its new agents committee, which selects novel unregistered anticancer agents for early clinical trials.
However, there are caveats, said Turowski. The preclinical study in rodents investigated only two parameters, of survival and satellite growth. "Survival would be a much more difficult outcome to measure in patients as there is huge variability. We are currently discussing with clinicians how best to test enhanced drug delivery in glioblastoma patients. So far we have not been able to come up with a satisfactory protocol. Nevertheless, we hope to be able to undertake some clinical test in the near future, and hope that this report will tempt others to do so, too," he said.
The research also is important in having enabled the development of a rat brain model that is amenable to detailed investigations of drug delivery across the BBB. "In fact we will submit a study later this year, which investigates a different mechanism of BBB opening in the same models. We have also looked at the transport of different classes of pharmaceutically useful agents," Turowski said.