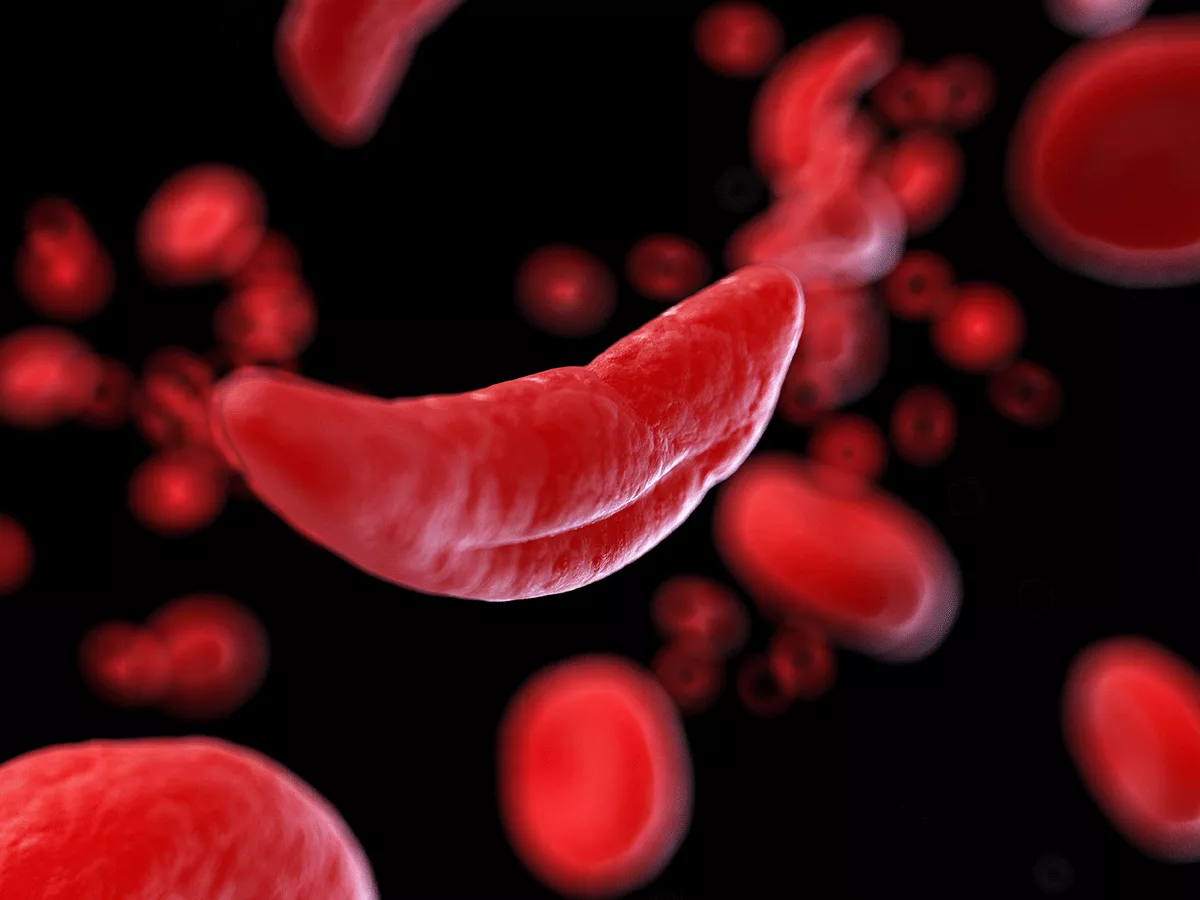
At the European Hematology Association's annual meeting in Vienna last week, companies reported impressive progress for the treatment of sickle cell disease.
Among intriguing results were those presented for Alexion Pharmaceuticals' ALXN-1820 indicating that cell-free heme is a potent trigger of complement alternative pathway activation in sickle cell disease and it can be blocked by targeting properdin. In red blood cells from patients with sickle cell disease, complement inactivated C3b (iC3b) and C5b-9 deposition resulted from exposure to heme and this was blocked by > 95% for iC3b and by > 85% for C5b-9 in the presence of ALXN-1820. Marked deposition of iC3b and C5b-9 was also observed in HMEC-1 endothelial cells exposed to heme, with deposition blocked by > 70% for iC3b and > 85% for C5b-9 in the presence of ALXN-1820.
Using the Townes mouse model of sickle cell disease, vaso-occlusion and hyper-hemolysis were induced by intravenous heme injection (50 mcmol/kg) or hypoxia-reoxygenation. Pretreatment with the mouse-specific properdin inhibitor 14E1 markedly ameliorated vaso-occlusion, reduced C3b and C5b-9 deposition on red blood cells and reduced hemolysis biomarkers. Targeting properdin with ALXN-1820 appeared to warrant clinical evaluation for acute and chronic sickle cell disease complications.
In other presentations, the high nonadherence rate and limited data on Fulcrum Therapeutics' phase Ib trial of oral fetal hemoglobin (HbF) inducer FTX-6058 make it impossible to tell, for the moment, whether the drug will reliably lead to clinically meaningful benefits.
Clearer evidence of benefit was observed in updated results on gene editing therapy Exa-cel (exagamglogene autotemcel, CTX-001; Vertex Pharmaceuticals/CRISPR Therapeutics). Exa-cel edits the Bcl11a locus to increase the production of HbF, which does not sickle.
In the 12 months after treatment with a single dose of CTX-001, none of the 31 treated patients had a vaso-occlusive crisis, while patients previously had a median of about 4 such crises per year.
Data were reported from the CLIMB-121 trial in sickle cell disease and the CLIMB-111 trial in transfusion-dependent thalassemia, where 42 of 44 treated patients did not need transfusions for a year after treatment. Up to 3 years of follow-up, the increase in HbF levels appeared durable, opening up the possibility of a one-time curative treatment. Exa-cel does require bone marrow conditioning with busulfan, and 2 thalassemia patients had severe adverse events related to the conditioning.
That was the background of the response that "personally, I'd rather have a pill than busulfan," given by Clark Brown when asked about the big-picture prospects of Oxbryta (voxelotor; Global Blood Therapeutics) follow-on GBT-601. Brown is associate professor of pediatrics at Emory University and presented data on GBT-601 at an oral session on Sunday.
Oxbryta, which is approved for individuals with sickle cell disease ages 4 and older in the U.S., and 12 and older in Europe and the United Arab Emirates, works by inhibiting polymerization. GBT-601 also inhibits polymerization but has improved pharmacokinetic properties compared to Oxbryta -- including, notably, an eightfold longer half-life -- enabling "higher hemoglobin occupancy at well-tolerated doses," Brown explained in his presentation.
The CTX-001 data, he said during the discussion, were "very encouraging, but we want to have a treatment that can be used for all patients, no matter where they live."
The question of access received broader treatment by David Rees, professor of pediatric sickle cell disease at King's College London, in his Sunday plenary session talk on "Precision Medicine in Sickle Cell Disease."
In one sense, he said, precision medicine is a fashionable term for an old concept -- "the same basic idea, that not everybody with the same condition is the same."
"Precision medicine is just medicine, really," he said.
But in terms of the evidence-based analysis that the term has come to signify, his take was that "there's really not much of it."
Partly, the reasons are related to research. The only well-validated prognostic risk factor is elevated blood flow velocity in the internal carotid or middle cerebral arteries as measured by transcranial doppler, which predicts an elevated stroke risk and is used as an indicator for blood transfusions.
Even here, though, "approximately 40% of children with abnormal dopplers wouldn't have strokes, and they are still transfused."
But research on other biological factors is largely lacking or, in some cases, is of poor quality. Biomarker studies, for example, can amount to fishing expeditions. Rees showed a study from his own lab that showed a statistically significant risk difference between Aries and Scorpio signs for complications of sickle cell disease -- nonsense, but the sort of nonsense that will inevitably pop up if enough post-hoc comparisons are run.
Another sobering issue is that for mortality from sickle cell disease, "the key factor is where you live. ... Environmental factors swamp genetic ones."
This is true globally, but also within high-income countries.
Clinical trials, at least, are increasingly run in the global malaria belt, where sickle cell disease is most known to confer a selective advantage and is most frequent. That change is a good thing in terms of research equity, but also means that therapeutics are tested in countries whose health systems cannot afford them. Rees called for "more sophisticated licensing arrangements, so the drugs are affordable in the countries where the diseases are common."