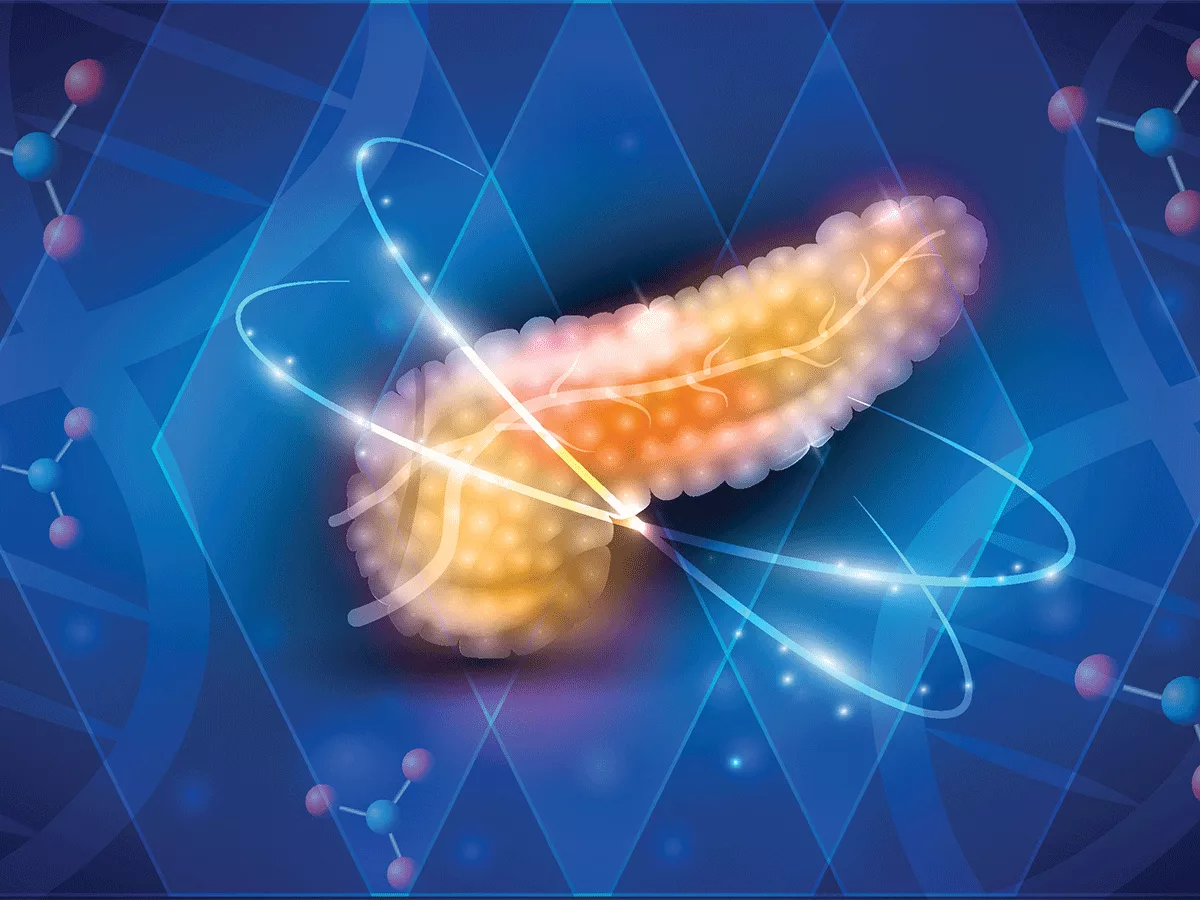
The growth of some pancreatic cancers is fueled by fungus-induced production of the cytokine IL-33, and the progression of such tumors could be slowed down by treatment with antifungals or genetic deletion of IL-33, researchers reported in the February 3, 2022, online issue of Cancer Cell.
The prognosis for pancreatic cancer patients remains among the most dismal of any solid tumor, with 5-year-survival rates barely out of the single digits.
In a grim irony, there are plenty of immune cells in pancreatic tumors. "Some of the tumors are 40-60% immune cells," Prasenjit Dey told BioWorld Science. Dey is an assistant professor of oncology in the Department of Immunology at the Roswell Park Comprehensive Cancer Center, and the senior author of the Cancer Cell paper.
However, those cells are type 2 immune cells -- TH2 cells and innate lymphoid cells 2 (ILC2) that stimulate tumor growth rather than killing cancer cells.
In the work now published in Cancer Cell, Dey and his colleagues first investigated what makes pancreatic tumors to the wrong kind of immune cells.
The answer turned out to be IL-33, a cytokine that attracts type 2 immune cells. The team showed that mutated KRAS increased the production of IL-33 by tumor cells.
IL-33 is a damage-associated molecular pattern (DAMP) molecule that is typically released by dying cells. But "IL-33 is not going to be released by the cancer cells, because they are not dying... There has to be something extrinsic that is causing the release," Dey said.
That extrinsic factor turned out to be certain fungal species that were present in the pancreas of tumor-bearing mice.
The team looked specifically at fungi because there is an established link between the fungal microbiome, IL-33, and more severe asthma.
When fungi entered the pancreas, which is normally a sterile organ, they stimulated pancreatic cancer cells to secrete IL-33. This, in turn, attracted types of immune cells that promote tumor progression, both by immune suppression and by metabolic reprogramming.
In animal models, both genetic deletion of IL-33 and treatment with antifungals extended the life of the animals, though targeting IL-33 had the larger effect of the two. Knocking out IL-33 more than doubled the animals' lifespans, from 30 day to between 60 and 80. Antifungal treatment added a more modest 10 days to the lifespan.
The findings are likely to be relevant beyond the specific KRASG12D mutation that Dey and his colleagues studied in their experiments, and possibly also beyond pancreatic cancer.
Although there are many different activating KRAS mutations, all of them activate the same downstream pathways, principally MEK-Erk and PI3K. In their studies, Dey and his team showed that IL-33 release appeared to be mediated through the MEK-Erk more than the PI3 kinase pathway.
The team plans to look at whether the same mechanism is at play in some cases of lung and colon cancer. While the pancreas is normally sterile, the lung and colon are organs that interface with the environment and have a microbiome while they are in a healthy state.
Clinically, the studies suggest that either antifungals or IL-33 targeting drugs might be useful in pancreatic cancer.
IL-33 monoclonal antibodies are in clinical development for asthma, and have been tested in other indications, though clinical results have been mixed.
Dey said that it is not clear yet whether the fungi colonize the pancreas, or whether invading fungi are killed by the immune system as they enter.
The team was able to find DNA and RNA from fungi in the pancreas, but not able to culture any fungi. It is possible that fungus is phagocytosed and presented by macrophages, in which case an antifungal drug would not be expected to have much of an effect on IL-33 production.
But the majority of microbes, be they bacteria, viruses or fungi, cannot be cultured with current technologies. And so another possibility is that the pancreas is colonized by fungi, but those fungi cannot be demonstrated at present.
Antifungals are an approved treatment for acute pancreatitis, so testing them in pancreatic cancer would be straightforward.