A Japanese study has discovered a new means of regulating endogenous gene expression in the CNS, using systemically administered antisense oligonucleotides (ASOs) in rodents, which facilitates development of ASO-based therapies for patients with neurological diseases requiring prolonged treatment.
The study demonstrated that cholesterol-functionalized DNA/RNA heteroduplex oligonucleotides (Chol-HDOs) could cross the blood-brain barrier (BBB) and knock down genes in the CNS of rats and mice, the authors reported in the August 12, 2021, edition of Nature Biotechnology.
"This is the first study to demonstrate that Chol-HDOs can cross the BBB and knock down genes in the CNS of rodents," said study leader Takanori Yokota, professor and chairman of the Department of Neurology and Neurological Science at Tokyo Medical and Dental University.
"This has major implications for managing neurological conditions requiring long-term ASO treatment, including Alzheimer's disease (AD), Parkinsonism, amyotrophic lateral sclerosis (ALS), multiple sclerosis, stroke and epilepsy," Yokota told BioWorld Science.
In patients with such CNS disorders, for example, lumbar puncture/intrathecal injection of ASO could be given to rapidly achieve therapeutic concentrations and regulate endogenous CNS gene expression, followed by maintenance therapy with intravenous or subcutaneous Chol-HDO injection.
Single-strand ASOs
Recently, single-strand ASOs have been extensively investigated for treating CNS disorders. For example, the ASO Spinraza (nusinersen; Biogen Inc.), which is approved for the treatment of spinal muscular atrophy, has been shown to modulate splicing of the SMN2 gene pre-mRNA.
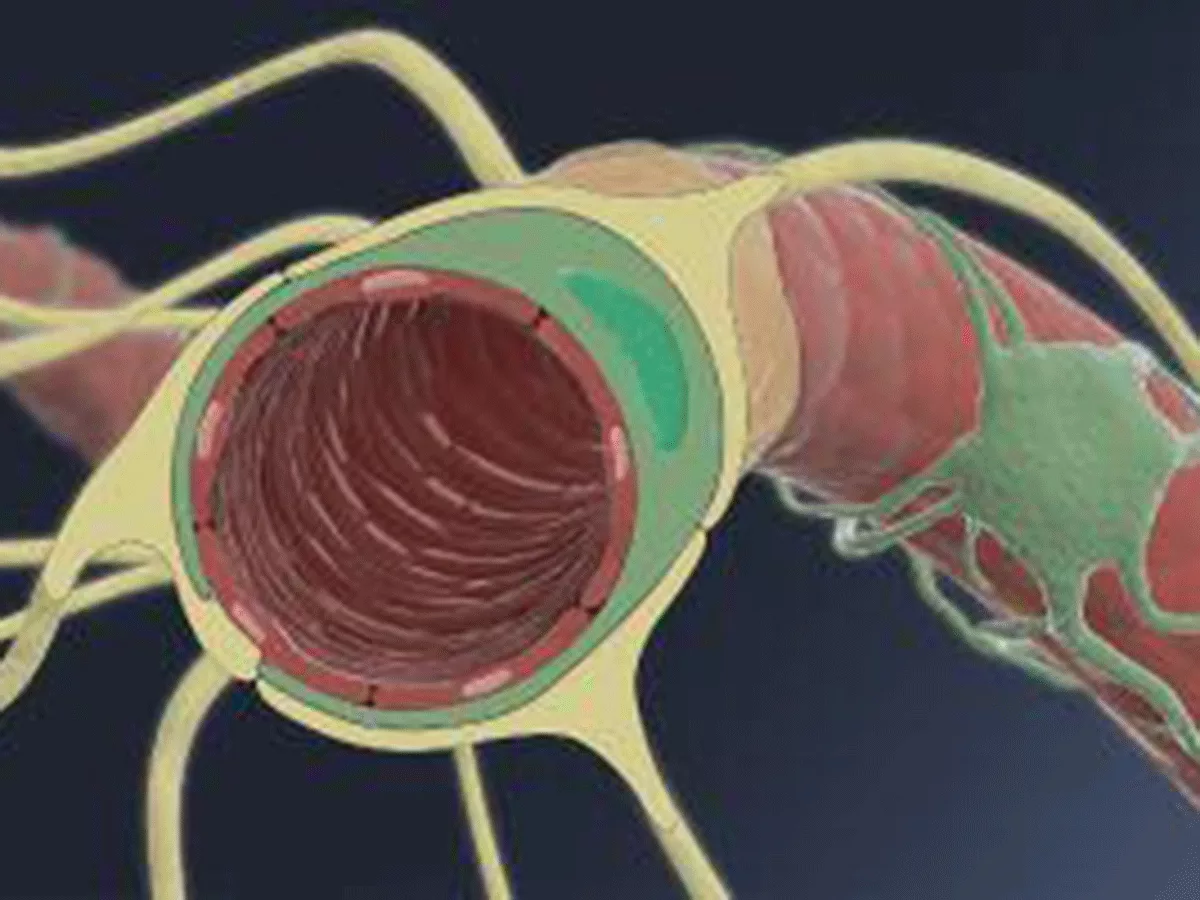
However, single-stranded ASOs cannot normally enter the CNS after systemic administration and must be intrathecally injected directly into the cerebrospinal fluid (CSF).
"Being highly polar, ASOs do not generally enter those brains with intact vascular barriers after systemic administration, without the use of treatments that open the BBB," noted Yokota.
In clinical practice, intrathecally injected Spinraza has been well tolerated by most patients, but can be difficult to use in individuals with severe lumbar scoliosis, or in combination with anticoagulant therapy.
Therefore, an effective method to deliver ASOs from the blood to the brain would be clinically advantageous.
An oligonucleotide-based drug to regulate gene expression in the CNS after systemic injection must be capable of crossing both the BBB and the blood-CSF barrier, which normally only small hydrophobic molecules can penetrate.
However, several recent strategies for delivering oligonucleotides into the CNS have not been proven to be effective.
For example, studies have shown that delivery of DNA/RNA HDO technology to the brain was negligible, despite its having been shown to enable efficient RNA degradation in the livers of mice and nonhuman primates when given via intravenous injection.
The authors of the new Nature Biotechnology study therefore sought to address this limitation by screening multiple lipid ligands that can conjugate with HDOs at a higher dose than that seen in previous protocols.
"Screening of approximately 60 different lipid ligands revealed that DNA/RNA HDOs conjugated to cholesterol or alpha-tocopherol could reach the CNS after subcutaneous or intravenous administration in rats and mice," said Yokota, noting, "this would allow patients to avoid the need for invasive lumbar puncture."
The HDOs were distributed throughout the brain, spinal cord and peripheral tissues and suppressed the expression of four target genes by up to 90% in the CNS.
"HDO distribution in the spinal cord was slightly higher than that in the cerebellum, with the greatest suppression being seen in metastatic associated lung adenocarcinoma transcript 1 (Malat-1) long noncoding RNA," said Yokota, noting that single-stranded ASOs conjugated to cholesterol showed only limited activity in this regard.
Furthermore, gene knockdown was seen in major CNS cell types, and was greatest in neurons and microglial cells, "suggesting this approach may be most effective in neuroinflammatory diseases including AD and ALS," said Yokota.
A potential safety concern of treating diseases with pathogenesis mainly restricted to the CNS is that biodistribution of Chol-HDO may be greater in peripheral tissues than in brain, potentially causing adverse side effects.
However, while doses needed to observe target knockdown in CNS with Chol-HDO were high, the compounds were generally well tolerated. Side effects such as thrombocytopenia and focal brain necrosis could be reduced by using subcutaneous delivery, or dividing intravenous injection doses.
These findings collectively show that by effectively crossing the BBB, Chol-HDOs can overcome the limited efficacy of ASOs targeting the CNS, without requiring invasive intrathecal administration.
Looking forward, said Yokota, "we will be working to enhance potency, which will involve ligand optimization of cholesterol and tocopherol derivatives, and identification of the specific molecular pathways underlying CNS delivery."