Science, BioWorld Science
Drug design, drug delivery & technologies
Pharma pools structural data to boost power of AI in drug discovery
Read MoreArtificial intelligence
New AI model simultaneously predicts risk of getting 1,000 diseases
Read MoreDrug design, drug delivery & technologies
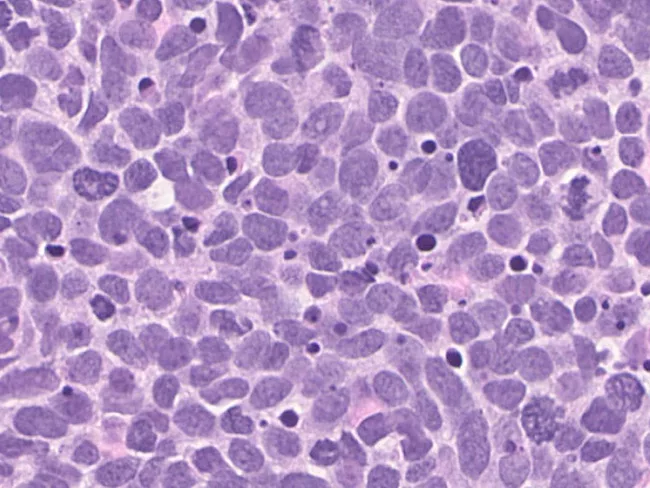
Cancer vaccines face collateral damage of mRNA funding cuts
Read MoreDrug design, drug delivery & technologies
Animosity toward mRNA COVID vaccines puts basic science at risk
Read MoreDrug design, drug delivery & technologies